
A discussion by county councillors about protective personal equipment needs in Kent has revealed the struggle being faced by care home staff and residents with one Thanet care home suffering a tragic 17 covid-related deaths, according to information shared with members of the authority.
Grosvenor Court in Cliftonville is a 62 bed residential home with staff trained in specialist needs, such as dementia care and learning disability, as well as sensory impairments and Parkinson’s.
The home, in First Avenue, falls in the Cliftonville West ward which has recorded the highest number of Covid-related deaths in Thanet with 13 registered up until April 17, far more than any other Thanet area.
Data for the loss of people to the virus at ward level has not been updated but information from the KCC virtual meeting last Friday, seen by The Isle of Thanet News, showed 17 people from the Cliftonville care home had lost their lives with covid being cited.
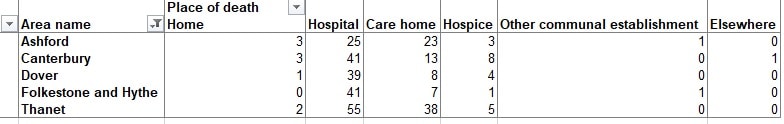
In Thanet as a whole there have been 100 covid-related deaths between March 2 and May 1, registered up to May 9, and 38 were in care home settings. Fifty-five were in hospital and two people passed away at home.
As concern over the plight of staff and residents at care homes across the UK grows, The Health Foundation also highlights how caring for people with dementia – which Grosvenor Court does – can add pressure.
The foundation said: “Outbreaks of infectious disease can be particularly challenging to manage in care homes. Residents may have dementia or other conditions that make isolating them particularly challenging, and infection control outside a hospital setting is difficult.”
Providing PPE

In a message to KCC Grosvenor Court owners Premiere Care Homes said in April ”things were really bad” and “at times we did not know where to turn” but guidance and support from the authority helping to source essential equipment had been beneficial.
KCC has been providing PPE for care homes, homecare providers, GPs and pharmacies with some 1,300 deliveries of 2.4 million items.
Some 276 care homes and 113 homecare providers have received PPE from the county council.
It comes at a cost to the authority, which has not charged for the PPE, with some £337,000 already spent and projections of circa £320,000 per week needed at current demand levels.
Carers on the frontline

Some in Thanet’s care home sector say supplies took too long to filter down to staff.
One carer from the isle said: “The homes I worked in didn’t receive any PPE until six weeks into the pandemic.
“One home is doing OK in terms of getting face masks but is now struggling to get gloves from their suppliers as they are still being directed to the NHS.
“I don’t feel safe, I feel the face masks that care homes have been provided with are inadequate. They are flimsy and quite frankly no different to having a t shirt over your face, they aren’t the 3m masks that the NHS have.
“They are literally just surgical masks that have probably no more than an hour’s life and yet we are expected to wear them for a minimum four hours at a time. They don’t seal on to the face at all.
“I worry after every shift that I might bring it home, it’s got to the point that I don’t want to go to work.”
However, other homes in Thanet have managed to get equipment after taking the decision to use their own funds.
Toni Selfridge, who is a manager alongside colleague Zoe Pitman at Newlyn residential home in Ramsgate, told The Isle of Thanet News: “If the owner hadn’t got the PPE themselves, we wouldn’t have received any.
“We have in the last two weeks been given visors and material masks and we did get one lot of masks at the very beginning.
“I’m 100% happy that we are safe. We were given numbers and an email address if we needed to get any more PPE and we have had so much support from the CCG and CQC.”
Toni said there had been no covid related deaths at the home she woks in and no positive virus diagnosis for any residents or staff.
She added: “I implemented infection control procedures. Staff come to work in civvies and then get their work clothes on when they get there. We have our temperature taken and anything over 38 means the person has to go home.”
One resident whose parents run accommodation for adults with learning disabilities said they had received no support to help keep people safe.
They said: “They have not had any support for the residents or themselves and no one provided them with PPE – they had to buy their own. It took four weeks for the PPE to arrive and the prices have sky rocketed.”
‘Stunned’

County councillor Karen Constantine, who sits on the authority’s health scrutiny panel, said: “I was stunned by the information which showed 17 deaths in an elderly care home in Thanet. The Guardian newspaper has described this poignantly as ‘kettled’ and certainly it’s true that the elderly in homes have zero choice about where they stay during this time.
“We know that this home is Grosvenor Court in Cliftonville and our thoughts are with the families and friends as they deal with their loss. I have to emphasise how hard staff are working there and that this isn’t their fault – they should not be blamed in any way.
“But the situation begs a vital and fundamental question about our elderly, shouldn’t they be completely safe? What about the staff and families of those connected to the home, have they now been tested for the virus? “
Councillor Constantine says she has asked county council leader Roger Gough a number of questions about Grosvenor Court, including what measures are now in place to both protect and reassure remaining residents and staff following such a traumatic experience.
She added: “I would like to know what financial support can be afforded to this home and others in similar circumstances, as such a terrible loss of life will undoubtedly have a severe detrimental financial impact too.
“We must do all we can as a county council to keep our businesses ‘standing up’ so that our residents are safe and cared for and the Government must be forced to underwrite the cost.”
A spokesperson for Premiere Care Homes said they were not currently in a position to comment, adding: “Our main focus at this present time is our care homes, our residents and our staff.”
National situation
Nationally, data from the Office for National Statistics shows the crisis is countrywide with 12,526 care home residents dying with covid cited or suspected between March 2 and May 1, registered up to May 9. Of these 8,312 deaths were in care homes with 4,214 residents dying in other settings such as hospitals.
Of the 12,526 deaths,11,371 were classified as “confirmed” COVID-19 and 1,155 were classified as “suspected” COVID-19.
Dementia and Alzheimer disease was the most common main pre-existing condition found among care home resident deaths involving COVID-19.
Government fund for care homes
Yesterday (May 15) the government announced a new £600 million Infection Control Fund to tackle the spread of COVID-19 in care homes, in addition to £3.2 billion of financial support made available to local authorities to support key public services since the start of the crisis.
The fund, which is ringfenced for social care, will be given to local authorities to ensure care homes can continue to halt the spread of coronavirus by helping them cover the costs of implementing measures to reduce transmission.
Care homes will be asked to restrict permanent and agency staff to working in only one care home wherever possible. The funding could be used to meet the additional costs of restricting staff to work in one care home and pay the wages of those self-isolating.
The money will be paid in two equal instalments to local authorities and sums are allocated according to the number of care home beds in each area.
For Kent, which has 14,579 registered care beds, the cash award is £18,877,765.

During yesterday’s briefing Secretary of State for Health, Matt Hancock, said two-thirds of care homes in England had not had any covid outbreak and that following the peak the number of new cases has now halved.
Further measures announced yesterday were:
- all local authorities must conduct a daily review of care homes in their area to ensure care homes have the support they need with staffing, help with accessing PPE and other areas of operation
- the NHS will ensure that each care home has a named clinical contact to provide better access to clinical advice through weekly check-ins to review their patients, and offer direct support for staff with use of equipment and medication
- a wellbeing package for social care staff is also being rolled out on the new CARE app including 2 new helplines, led by the Samaritans and Hospice UK. This will help support care staff with their mental health and wellbeing and support those who have experienced a traumatic death as part of their work or help with anxiety and stress
ONS data shows people working in social care, a group including care workers and home carers, both had significantly raised rates of death involving COVID-19, with 131 deaths recorded up until April 20. This figure will have likely increased since that data was released.
A new online portal that makes it easy for care homes to arrange deliveries of coronavirus test kits was also launched on May 4.
All care home staff and residents in England are now eligible for testing and this will be prioritised for care homes that look after the over 65s.

