
Health campaigners are making a last stand as a decision by health chiefs to close QEQM Hospital’s acute stroke service in favour of a hyper-acute unit in Ashford is taken this afternoon (February 14).
A final decision on the location for three units across Kent & Medway is expected to be confirmed by the Joint Committee of Clinical Commissioning Groups at the meeting taking place now in Maidstone.
The proposed shortlist was announced at the start of last year. The preferred option was then confirmed in September as Darent Valley Hospital, Maidstone Hospital and William Harvey Hospital.
The plan is for Darent Valley to have a 34 bed unit, Maidstone General Hospital 38 beds and William Harvey Hospital 52 beds. There will also be a two bed outflow at Eastbourne General Hospital.
There will be no acute stroke services at Medway Hospital, Tunbridge Wells Hospital, Margate’s Queen Elizabeth the Queen Mother Hospital and Kent & Canterbury Hospital – which has already had its service withdrawn due to the removal of training doctors by Health Education England in March 2017
The JCCG expects the hyper-acute units at Darent Valley and Maidstone to go live in March 2020 followed by the William Harvey Hospital in spring 2021.
Thanet campaign

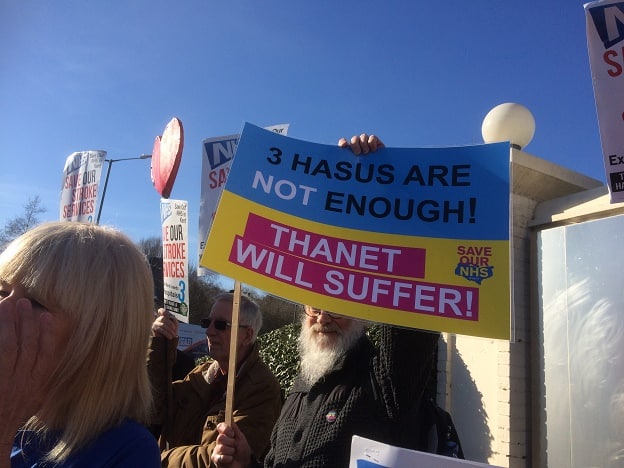
Thanet campaigners have been fighting the proposals, saying isle lives will be at risk because of the journey times to Ashford which take more than one hour from Thanet.
Calls have been made by the Save Our NHS in Kent group for the Kent and Medway NHS to look at the proposals again to include a fourth HASU unit at the QEQM.
Campaigner Carly Jeffrey said: “The final decision on the NHS stroke proposals to close three of the six stroke units in Kent & Medway rests with 20 GPs, who will vote to pass the plans through or vote against to reject.
“If they vote for the plans, then the stroke units in Margate’s QEQM hospital, at Medway Maritime Hospital and Pembury Hospital will close. Stroke sufferers in Thanet will have to travel over an hour to Ashford for treatment, on top of 40 minutes for ambulance delays for 10% of patients. This is absolutely unsafe as stroke requires the most urgent attention.
“We must make these GPs understand the dangerous consequences of their decision for the people of Thanet. “

A JCCG report says East Kent Hospitals University NHS Foundation Trust (EKHUFT) concluded that it would not be possible to run two Hyper Acute Stroke Units because it would be very difficult to deliver due to recruitment issues and the risks around staff relocation. Of the sites run by the trust (QEQM, William Harvey and Canterbury), the William Harvey Hospital was identified as the best option for a hyper acute stroke unit.
It is planned provide additional funding of £500,000 per year for the ambulance service which will ‘upskill’ paramedics. The JCCG say there will also be an increase in specialist stroke staff including an estimated 8.8 additional consultants, up to 107 additional nurses and 46 additional physiotherapists and occupational therapists.

The report adds that the units will reduce financial deficits in the Kent and Medway service, although a review of those finances will take place.
An estimated £13.6m was spent by CCGs on acute stroke activity in the Kent and Medway catchment area in 2016/17. Hospital stroke services are currently running at an estimated £7.5 million deficit. The new service would decrease that deficit by £0.5m
The cost to CCGs of implementing the new hospital stroke service model has been estimated at £3m per year :
- An estimated £1.7m, comprising the costs of re-training the work force, double running, excess travel and agency premium to continue services on those sites set to cease services.
- An estimated £1.6m costs for agency premium to continue services on those sites set to cease services.
- A proposed annual £0.5m (full year effect) increase in ambulance costs reflecting the impact of the increase in ambulance mileage.
- Plus a £3.3m for programme management costs to implement the changes and three years for the renting of a modular building in Dartford
These costs are in addition to a total capital investment of £27.7million
The JCCG say current units are understaffed with QEQM having a shortfall of 4 specialist consultants.

