
A shocking shortage of GPs, nurses, therapists and specialised medical staff is one of the driving forces behind proposals to change community health and hospital services in Thanet and across Kent and Medway, a meeting in Ramsgate was told last night (November 13).
The NHS listening event, held to discuss two options for the future of hospital services in east Kent and plans to expand community services, attracted a full crowd of some 50 people to the Pegwell Bay Hotel.
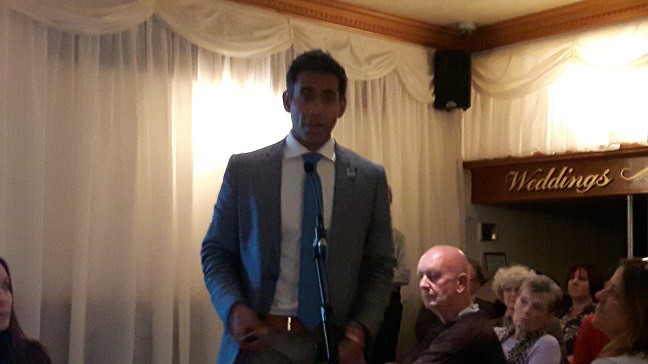
Dr Jihad Malasi, chair of NHS Thanet Clinical Commissioning Group (CCG) which commissions health services, told the gathering that a better use of the workforce, more delegation to other trained staff and centralisation of specialist services was the way forward.
He said: “Things have to change and it has to do with workforce ratios and the number of doctors we have. Even if money was available on tap we still would not have the workforce we need. That’s why we need to restructure.”
Dr Malasi said some GP practices were also unable to sustain themselves financially, with closures on the isle meaning surgeries had dropped from 17 to 13 in just 18 months.
He said: “Many of them have not been able to get the right staff and they have not been able to get locums. This is why we have to look very carefully at how we deliver things.”
He added: “Many GPs are burning out or are over a certain age. Demand on practices in phenomenal. We love our patients and love seeing them but when dealing with that level of demand it is difficult not to see people burning out.”
The meeting was told expanded community services and the use of response teams would also relieve pressure on hospitals.
In the second half of the meeting the discussion turned to proposals to centralise A&E and specialist services such as emergency stroke response, heart attacks, births with complications and some child inpatient care, to one major hospital.
Options put forward are:
Option 1
- A bigger, modern, A&E at William Harvey Hospital, Ashford, which would also provide services for people that need highly specialist care (such as trauma, vascular and specialist heart services) in east Kent
- an expanded, modern A&E at Queen Elizabeth the Queen Mother Hospital (QEQM), Margate, with inpatient care for people who are acutely unwell, emergency and day surgery, maternity and geriatric care
- investment in beds and services at Kent and Canterbury Hospital which would have a 24/7 GP-led Urgent Treatment Centre, and services including diagnostics (such as X-ray and CT scans), day surgery, outpatient services and rehabilitation.
Option 2
- the fitting out of a new build and refurbishment of some of the current buildings connected to the Kent and Canterbury Hospital, which would provide a single 24/7 A&E and all specialist services (such as trauma, vascular and specialist heart services) for the whole of east Kent
- QEQM Hospital and William Harvey Hospital would have 24/7 GP-led Urgent Treatment Centres, as well as diagnostics (such as X-ray and CT scans), day surgery, outpatient services and rehabilitation.
Developer Quinn Estates has offered to donate to the NHS land and the shell of a new hospital, as part of a development of 2,000 new homes, which includes an access road from the A2. It would be subject to planning permission.

East Kent Hospitals Chief Executive Susan Acott said the plan was for all three hospitals to specialise in some area and for at least one to take on planned care, such as pre-booked operations which would not be disrupted by the need for emergency beds.
She said: “East Kent has a lot of specialist services that lots of other parts of the county and country do not have. We have to support that work so it stays in east Kent and does not go to London. We cannot make the assumption that we can keep all the specialist services we have now, we make an investment in them.”
But the lack of a third option for A&E at all three main east Kent hospitals and a preferred option to move emergency stroke services to a hyper-acute unit at Ashford’s William Harvey Hospital raised a lot of angry questions from the crowd.

Carly Jeffrey, from campaign group Save Our NHS in Kent, said: “People should not have to travel for more than 30 minutes to A&E, often on bad roads. Anyone who lives here know the journey (to Ashford) is very difficult.”
Ms Jeffrey said data used to suggest two A&Es for the area rather than three was based on out of date information which had been superseded by reports stating that there was no evidence showing that centralisation of services is beneficial, particularly in a wide-ranging, partly rural area such as Kent.
She added: “We need a third option included next year when this goes to consultation. We have no option for three A&Es and are being told it is not viable but it should be included. There should be a list of pros and cons for each option in the documentation. (The NHS) must trust the public to make a good choice.”
County councillor Karen Constantine, who sits on the authority’s health scrutiny committee, said she agreed with moving more health work into the community and keeping people in their own homes when possible but questioned how the shortfall of staff and funding would be met.
She said: “I would really like to back the proposals. But I cannot see how we can deliver what’s needed without much more cash and a realistic plan to address the massive workforce issues.
“I’m not convinced these changes aren’t being driven by money. And that’s simply not right.
“It’s absolutely clear to me the NHS cash crisis is creating a workforce crisis.”

Mrs Selkirk denied the proposals were purely down to finances and said it was about having a viable workforce.
A final decision on whether emergency stroke services will be moved to Ashford, with QEQM retaining its rehabilitation work, will be made in January next year.
However Mrs Selrkirk admitted the two option proposal for the overhaul of east Kent’s hospitals could take as long as ten years to implement.
She said: “This will take quite a number of years, between five and 10 and most likely at the 10 year end.
“We need to consider how to manage services in the interim, such as community care and managing services safely. Neither option can be delivered in a short period of time.”
The next steps will be an evaluation of the options and a confirmation of a shortlist. A pre-consultation business case will then be prepared and go before a South East Clinical board. It then has to be reviewed by NHS England.
If it is given the green light the proposals will then go to public consultation, a preferred option will be confirmed and a full business case made. Only after this stage can the plans actually begin to be put into practice.
Another listening event takes place in Margate on Tuesday 20 November from 9:45am to 1pm at the: Global Generation Church, Unit 2, Westwood Business Park, Margate, CT9 4JJ.
Labour Councillors will be holding a candlelight vigil on November 22. 3pm-6 pm, outside Thanet council’s offices in Margate in protest at the health proposals.
A survey to submit has been extended until December 7 and can be found at https://www.smartsurvey.co.uk/s/EastKentNHS2018/
SONIK
Find a Sonik petition for three east Kent A&Es here
Find the group on facebook at https://www.facebook.com/SaveOurNHSKent/

