East Kent Hospitals Trust (EKHUFT) has pledged to put more improvements in place to ensure safe, high quality maternity care for women and their families and to learn the lessons from past failures.
The trust has published an ‘Excellence in Maternity Care’ strategy outlining how it plans to make the service better.
The plan focuses on five areas – women and families; quality and safety; staff; the future and sustainability.
Amongst the promises made are making sure staff have the time, skills and training to carry out their roles; improving access and reducing inequalities in experiences, quality and outcomes of care for those women at highest risk of poor outcomes; putting in place actions to improve women’s health before, during and after pregnancy; improving facilities and to be open when things do not go as planned.
Last year the Care Quality Commission (CQC) rated maternity services provided by East Kent Hospitals Trust as Requires Improvement. Two Requirement Notices were also issued relating to improvements needed to governance and provision of the safe care and treatment in maternity services.
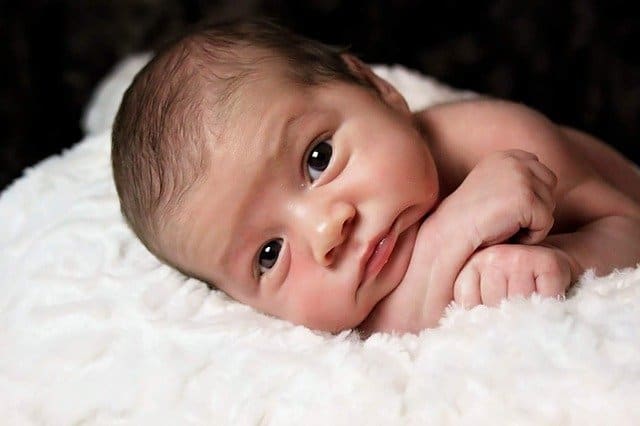
The CQC inspections took place after concerns were raised about the safety of maternity services at the Trust, including during an inquest that January into the death of baby Harry Richford, at Queen Elizabeth The Queen Mother Hospital in 2017. A number of families then came forward over the preventable deaths of their babies and, in October 2020, the CQC confirmed it was prosecuting the trust on two offences of failing to provide safe care and treatment.
Recommendations made by the coroner at Harry’s inquest have now been implemented, the Trust says.
Special measures and reviews
Issues with the service go back further to August 2014 when the Trust was placed in special measures by the CQC. At the time of that inspection maternity services were rated as ‘Requires Improvement’ overall.
The CQC noted a lack of leadership, equipment shortages and a culture of bullying and harassment. During that CQC visit the maternity unit at Margate, though rated ‘Good’ for caring, was rated ‘Inadequate’ for safety. Between that CQC visit and the subsequent CQC inspection, in July 2015, there were some improvements but the CQC still rated the Margate maternity unit as ‘Requires Improvement’ with similar themes to the earlier inspection.
An independent review of maternity services was carried out by the Royal College of Obstetricians and Gynaecologists (RCOG) at the end of November 2015.
The RCOG report highlighted issues including a lack of reviews for high risk women at QEQM and a reluctance to attend out of hours calls at the same site.
The report examined seven cases where serious incident reviews had been carried out. Two of these involved the death of babies. Another 16 cases included mothers developing severe pre-eclampsia.
In 2016 the Trust introduced measures including more consultants on hand during births, investment in equipment and training on identifying and safely supporting difficult births for all maternity staff. In 2018, the Trust restructured its maternity service into a clinically-led service and a new Head of Midwifery was appointed in 2019.
The troubled maternity service has also been subject to a report by the Health and Safety Investigation Branch (HSIB) which found recurrent patient safety risks and it is subject to a review commissioned by NHS England and NHS Improvement into the maternity and neonatal services. That investigation is being led by Dr Bill Kirkup and is expected to cover the period since 2009. Dr Kirkup expects to report his findings this year. It is thought that as many as 40 families have come forward to the review with concerns.

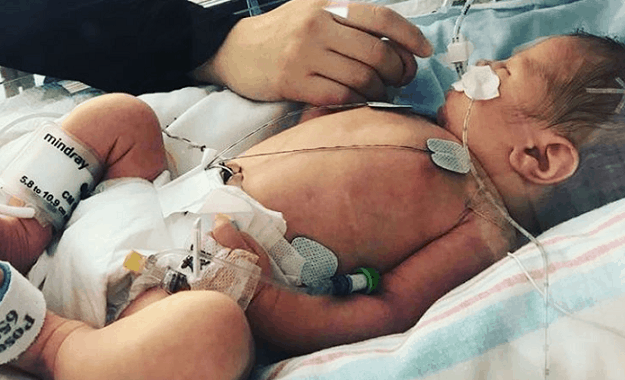
Last year the Trust also admitted failings following the death of five week old Luchii Gavrilescu in December 2019 which would have been preventable if action to diagnose and treat his father for tuberculosis (TB) had been taken almost two years before.
A full inquest into Luchii’s death is due to be held.
In 2019, the Trust implemented further improvements with a more comprehensive way of monitoring the fetal heart during labour and appointing two new specialist, fetal wellbeing midwives.

EKHUFT chief exec Susan Acott said of the new strategy: “Our strategy is one of continuous improvement, creating the right environment for our staff to be able to implement best practice and to have the confidence to raise concerns when standards are not being met. It’s our commitment to the women and families of east Kent to work tirelessly to provide high quality maternity care, which is safe, effective and centred on the women that need it.
“Our strategy incorporates the recommendations from independent investigations, findings and feedback into maternity care at East Kent Hospitals to ensure the recommendations and lessons learned from these are fully embedded. This includes the NHS England maternity support programme, NHS Improvement, the Care Quality Commission, Kent and Medway Clinical Commissioning Group, Kent and Medway Local Maternity Systems, the Maternity Voices Partnership and Healthwatch Kent.
“We are determined that we will be open and transparent about the improvements we need to make to our maternity service. We have already made a number of improvements, but we are clear that more needs to be done.
“We have listened to women and families – to those who have received excellent care, and those we have failed by not providing the right standard of care. To these women and families we are profoundly sorry.
“We have also listened to the views of our own multi-professional staff on what values and skills they need to be equipped with, in order to deliver a safe high quality service.”

County Councillor Karen Constantine, who is on the authority’s health scrutiny committee, said the improvement plan was overdue but welcome.
She said: “QEQM has suffered from a poor reputation with regard to its maternity services for a long time now. This report and its recommendations are long overdue but are very welcome.
“Some of the issues raised in the report, such as measures of deprivation, are beyond the scope of the NHS to deliver improvements on. Central Government must act and our local MP needs to grasp the importance of these issues and lobby his Government. This is vital if we are ever going to see safe and adequate maternity services in Thanet.
“I am further concerned about any potential NHS reorganisations that could see maternity services moved away from Thanet. Labour will vehemently oppose any plans to remove maternity services from Thanet women.”
The improvement report highlights poor maternity/birthing outcomes for those in deprived areas such as Thanet where there is a higher prevalence of smoking, alcohol intake, drug use, obesity, and malnourishment.
Cllr Constantine added: “There is no doubt in my mind that with poverty and child poverty soaring unchecked in Thanet, the necessary delivery of improvements in maternity will be incredibly difficult to deliver. I admire the ambition and dedication of our NHS staff in their efforts to ensure better births for everyone becomes a reality in Thanet.
“We also will continue to struggle to deliver better maternal mental health services whilst we are also dealing with the on going impact of Covid.
“The additional key issue is workforce. Without an adequate number of well trained and well supported clinical staff, midwives and midwife support workers these targets cannot be met.
“The Royal College of Midwives has recently published research which showed eight out of 10 (83%) members say they do not feel their maternity service has the right number of staff to operate safely, with a further 71% of members considering leaving the profession for good. This is a stark warning that midwives will leave the profession in their droves if they are not awarded a decent increase in pay.”
Cllr Constantine says NHS staff are doing their best under challenging circumstances but need to receive good pay and terms and conditions of employment. She said closer attention also needs to be paid to the link between poverty and poor health outcomes such as still births, low birth weights, and maternal mental health.

